Ten-year outcomes of M-MIST
therapy for intrabony defects with
and without regeneration materials
Authors:
Pierpaolo Cortellini, Simone Cortellini, Daniele Bonaccini, Maurizio S. Tonetti
Background
Clinical outcomes of periodontal regeneration are obtained
by applying different surgical techniques and regenerative
materials.
Surgical techniques have become efficient because of the
adaptation of modified incisions to preserve the interdental
tissue. These techniques are designed to maintain the integrity
of the papilla to allow better wound closure, protection of the
coagulum, and first-intention healing.
Enamel matrix derivative (EMD) and resorbable membranes
are the “gold-standard” materials for deep intrabony defects in
combination with deproteinised bovine bone mineral (DBBM)
for non-supporting defects.
To reduce the flap dimensions, healing time, and patient
discomfort, and to improve wound stability, minimally invasive
surgical approaches have been introduced, such as the
modified minimally invasive surgical technique (M-MIST) and
the single-flap approach (SFA). Although minimally invasive
surgical approaches – with and without biomaterials – for
treating intrabony defects have been compared, the long-term
stability of the outcomes had not been explored before.
Aim
The aim of this study was to compare the clinical stability of
treatment with the M-MIST technique, alone and in combination
with two different regenerative approaches in intrabony defects,
and to evaluate the costs of reintervention required over a 10-
year period.
Materials & methods
• A 10-year follow-up of a randomised controlled trial comparing three
different modalities in deep intrabony defects: M-MIST alone, M-MIST
+ EMD, M-MIST + EMD + DBBM.
• Forty-five participants presenting one deep intrabony defect, located
in the inter-proximal area and not extending into the furcation area.
• Patients were randomly assigned to one of the three treatment
groups: (i) M-MIST alone (n=15), the suture was tightened
to have blood-clot stability; (ii) M-MIST + EMD (n=15),
ethylenediaminetetraacetic acid (EDTA) was applied for two minutes
before applying EMD; (iii) M-MIST + EMD + DBBM (n=15), EDTA and
EMD were applied before DBBM was placed.
• Clinical measurements –plaque scores, bleeding on probing,
pocket probing depth (PPD), and clinical attachment level (CAL)–
were evaluated one week before surgery and at the follow-up
examinations.
• Radiographic examinations –distance between the cementoenamel
junction and the bottom of the defect [CEJ-BC] and distance between
the cementoenamel junction and the tooth apex [CEJ-A]– were
performed with an electronic ruler one week before surgery and at the
follow-up examinations.
• Long-term supportive periodontal care (SPC): patients were enrolled
every three months and, in case of disease recurrence, non-surgical
root debridement, access-flap surgery, or regenerative surgery were
Figure 1: Complication-free survival
Figure 1: Complication-free survival
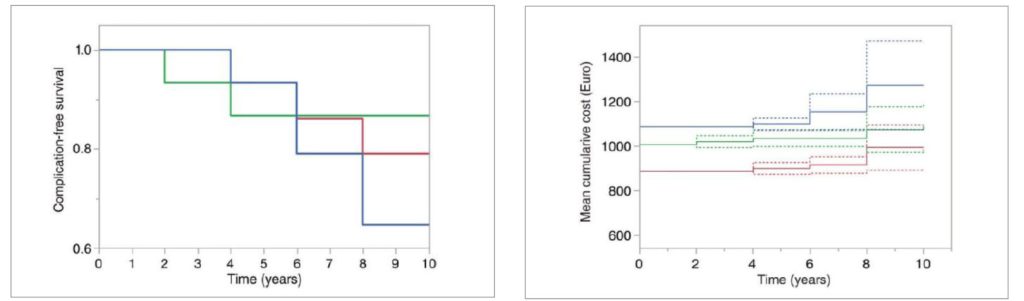
Mantel-Haenszel complication-free survival curves for the three groups
(modified minimally invasive surgical technique [M-MIST] in red,
M-MIST + enamel matrix derivative [EMD] in green, and M-MIST + EMD +DBBM
in blue). The diagram shows the interval until the first recurrence of
periodontitis event observed at the experimental teeth. No significant
differences were observed between groups.
Mean cumulative cost of recurrence (in euros) over the 10 year
observation period. The diagram shows all periodontitis recurrence
events observed and the actual cost of management of the recurrence
and includes the cost of surgical treatment. The dashed lines represent
the 95% CI. M-MIST is in red, M-MIST EMD is in green, and M-MIST
EMD DBBM is in blue.
Results:
Experimental population:
• Three subjects were lost to follow-up for reasons unrelated to
treatment: one in each group –two after four years and one after six
years.
• The sample was considered homogeneous as no differences
between groups were observed regarding the full-mouth plaque and
bleeding scores at different time points.
• All subjects were compliant regarding SPC.
Clinical and radiographic outcomes:
• No significant intergroup differences were observed at baseline,
one year, and 10 years regarding CAL, PPD, and radiographic
bone-level changes.
• Intragroup differences were significant between baseline and one
year, but no significant changes were observed between one year
and 10 years.
• Study had 13.3% power to detect a 0.2mm intergroup difference in
CAL between the one- and the 10-year follow-up (ANCOVA).
Complication-free survival:
• Ten events requiring additional periodontal therapy were observed:
three in the M-MIST group, five in the M-MIST + EMD + DBBM
group, and two in the M-MIST + EMD group. The respective
survival until the occurrence of the first event requiring additional
periodontal therapy beyond regular SPC was four years, four years,
and two years.
• No significant differences in complication-free survival between the
three groups were observed, which was 7.46 years (95% CI: 7.05-
7.87) for the whole population.
Mean cumulative cost of recurrence:
• Without including the surgical cost, the group with the highest cost
of managing disease recurrence was the M-MIST + EMD + DBBM
group.
• The cost of the global treatment, including surgical cost and the
cost of recurrence management, was also higher for the M-MIST +
EMD + DBBM group.
Limitations
No information was
given on whether
the periapical
radiographs were
standardised or not.
• Statistical power may
benefit from bigger
sample groups.
Conclusions & impact:
• Teeth presenting intrabony defects associated with deep pockets can be successfully treated with
an M-MIST approach, with or without regenerative material.
• Avoiding regenerative material provides the same short- and long-term benefits at lower cost,
compared to a regenerative approach with biomaterial.
• If the patient is compliant with the SPC programme, treated teeth can be maintained over 10 years.
• Avoiding regenerative materials in the M-MIST technique for treating intrabony defects can provide
satisfactory survival at a lower cost.