Background
Peri-implantitis is a plaque-associated pathological condition affecting the tissues around dental implants. It is characterised by inflammation in the peri-implant mucosa and progressive loss of supporting bone. Reported risk factors include poor oral hygiene, a history of periodontitis, and irregular supportive therapy.
It has been suggested that there may be an association between certain prosthetic features and peri-implantitis. It has been argued that a straight emergence profile or concave interproximal areas can facilitate oral-hygiene measures at fixed dental prostheses, while over-contoured restorations may interfere with the periodontal health of natural teeth. The same may be true for implant-supported prostheses.
In fact, suboptimal access for proper plaque control is a common finding in peri-implantitis cases. A prosthetic design with a small emergence angle and a straight or concave emergence profile may facilitate self-performed plaque control and thereby minimise the risk of marginal bone loss and peri-implantitis. It is therefore worth investigating the influence of various prosthetic features on the risk of marginal bone loss and peri-implantitis.
Aims
The objective of this study was to analyse the impact of various prosthetic features and other known risk factors on the prevalence of peri-implantitis by building a prediction model.
Materials & methods
• This is a cross-sectional study on patients who had received dental-implant restorations between March 2002 and February 2012 in a university clinic in Seoul, South Korea.
• Exclusion criteria included patients who had systemic diseases and conditions, who had irregular maintenance care or poor oral hygiene, who were smokers, or who had been treated previously for peri-implantitis.
• Implants from different manufacturers with various implant connection types were included (bone-level external, bone-level internal, and tissue-level).
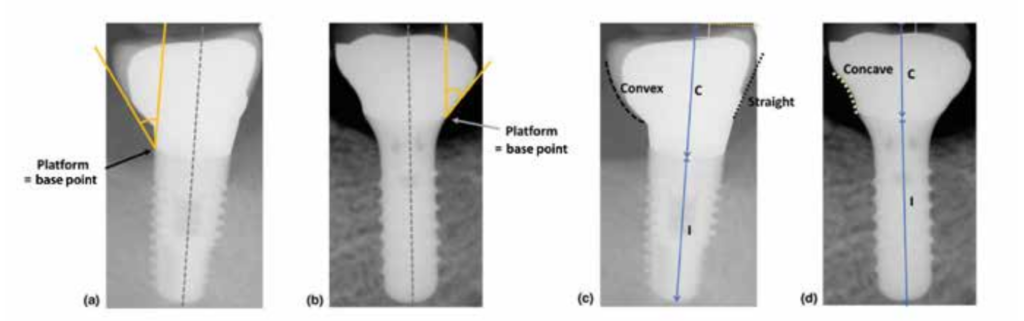
• Data was categorised according to the implant-connection type (bone-level external, bone-level internal, or tissue-level),
emergence angle (above and below 30 degrees), emergence profile (concave, straight, or convex), implant location, implant
diameter and length, history of periodontitis, bone augmentation, immediate or deferred implant placement, one- or two-stage protocol, screw- or cement-retained, implant position within the restoration (single, splinted mesial, splinted middle, splinted distal), and crown/implant ratio (see figure).
• The case definition for peri-implantitis was presence of bleeding on probing (BoP) and/or suppuration, increased probing depth, and bone loss > 0.5mm as measured on the radiographs one and five years after the insertion of the prosthesis.
• Marginal bone loss and the prosthetic features were measured on intra-oral radiographs obtained using the paralleling
technique. Marginal bone loss, the emergence angle, and the emergence profile were assessed on the mesial and distal
aspects.
Results
• The study included 169 patients with 349 dental implants.
• 173 of 349 implants were diagnosed with peri-implantitis.
• At tissue-level implants (6.3% of all implants), the effect of the analysed factors on marginal bone loss and the prevalence of peri-implantitis was not statistically significant.
• At bone-level implants, there was more marginal bone loss and peri-implantitis was found more frequently compared to
tissue-level implants. Marginal bone loss and prevalence of peri-implantitis were higher with external types of connection, an emergence angle ≥ 30 degrees, and a convex emergence profile.
• The risk of marginal bone loss and peri-implantitis was higher for implants in a middle position in a bridge compared to other positions.
• The risk of peri-implantitis was highest when a combination of an emergence angle of ≥ 30 degrees, a convex emergence profile, and a splinted-middle position was present (OR 287).
• Other factors –such as a history of periodontitis, crown/implant ratio, and screw- or cement-retention of the prosthesis–
all had an effect on marginal bone loss, but the effect was not statistically significant for the current presence of periimplantitis.
• For the final prediction model, only emergence angle, emergence profile, and splinted position within the restoration had enough sensitivity and specificity to be included.