Does a collagen matrix add
dimensional stability in guided
bone regeneration?
Authors:
Goran I. Benic, Stefan P. Bienz, Young Woo Song, Jae-Kook Cha, Christoph H.F. Hämmerle, Ui-Won Jung, Ronal
Background
In cases where there is insufficient bone availability to place
implants, guided bone regeneration (GBR) simultaneous
with implant placement is commonly used. It is usually
performed with particulated grafting materials and resorbable
membranes, as explained by the systematic review published
in 2019 by Thoma et al. However, both this review and other
studies showed how the combination of these materials for
successful regeneration was sometimes not predictable and it
was not adequate in the case of non-contained bone defects,
mainly because of their lack of dimensional stability.
As a result, different materials have been developed to
increase dimensional stability, such as the soft-type block,
which consists of a mixture of particles of bone substitutes
in a collagen matrix. This combination was developed for
alveolar ridge preservation (ARP) because of its increased
ability to maintain the augmented space and the ridge
contours, as was shown in the results of two in vitro studies
(Mir-Mari et al., 2016, 2017).
However, there is still not enough evidence from in vivo preclinical
and clinical studies, especially regarding the long-term
results when using these materials.
Aim
The aim was to compare the hard-tissue dimensions and
dimensional stability after guided bone regeneration of periimplant
defects, using either a soft-type block-bone substitute,
in which the bone substitute was incorporated into a collagen
matrix, or a particulated bone substitute.
Materials & methods
• This prospective randomised clinical trial included 40 patients
in need of at least one dental implant and simultaneous bone
augmentation of peri-implant defects, with a follow-up of six months.
Conventional inclusion and exclusion criteria for implant therapy were
applied, and heavy smokers were excluded.
• Forty patients were randomised into two parallel treatment groups.
Patients in the control group received a particulate synthetic biphasic
calcium phosphate (BCP), comprising 60% hydroxyapatite and 40%
beta tricalcium phosphate (HA/TCP), whereas those in the test group
received a soft-type block bone in which the same synthetic BCP
was embedded in a collagen matrix (CM) to improve its dimensional
stability.
• Implants were placed at least two months after tooth extraction,
leaving peri-implant bone defects that were filled and overaugmented
with the material during the surgery. Bone dehiscences
were classified in contained and non-contained defects, and their
apicocoronal dimension was measured on the buccal implant
surface. Local antiseptics and systemic antibiotics were prescribed
during the healing period.
• Re-entry surgeries were performed six months after implant
placement, and the residual presence of bone dehiscences was
measured, along with other clinical parameters.
• Cone beam computed tomography (CBCT) scans were performed at
baseline, immediately after implant placement, and after six months,
and assessed by a blinded investigator. The horizontal dimension
of the augmented bone at the implant shoulder was evaluated and
considered as the primary outcome variable for sample calculation.
• Other radiographic variables such as the vertical and diagonal
dimension of augmented bone were also evaluated at the various
time points.
Does a collagen matrix add
dimensional stability in guided
bone regeneration?
study
Authors:
Goran I. Benic, Stefan P. Bienz, Young Woo Song, Jae-Kook Cha, Christoph H.F. Hämmerle, Ui-Won Jung, Ronald E. Jung
Figure: Complete clinical sequence of each treatment modality with full defect resolution
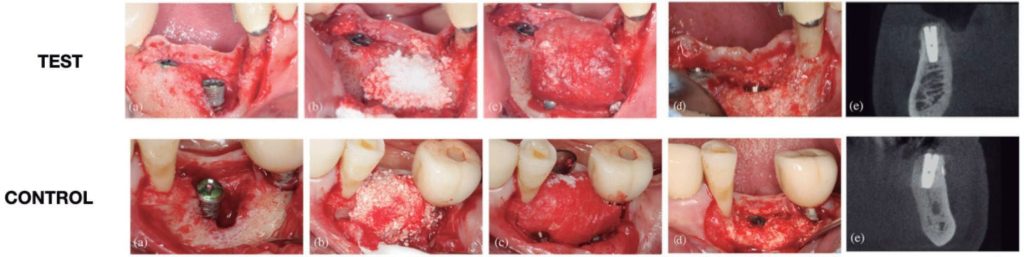
Baseline situation after implant placement (a), guided bone regeneration with the selected bone graft (b), collagen membrane stabilised (c),
complete defect resolution at re-entry surgery (d), and CBCT six months after implant placement (e).
Results
• Thirty-five subjects were finally included in the six-month analysis
(17 in the test group and 18 in the control group).
• With regards to soft-tissue dehiscences, only one was found in each
group.
• Horizontal hard-tissue dimensional changes, measured by CBCT,
showed mean augmentation values of 1.15mm (test) and 0.93mm
(control), with no statistically significant differences.
• When clinically measuring apicocoronal hard tissue changes at
the re-entry surgery, 58.8% of the test sites and the 55.6% of the
control sites, showed a complete vertical defect fill. When assessed
by CBCT, higher percentages of complete vertical defect fill were
observed (82.4% for the test group and 88.9% for the control group).
• Combining both groups, 14 contained and 21 non-contained defects
were included. At six months, only two of the 14 contained defects
(7.1%) did not achieve complete vertical fill (both in the control
group); while 13 out of 21 (61.9%) non-contained defects did not
achieve complete vertical bone fill, with similar results in both
groups – 58.3% (test) and 66.7% (control).
• In both type of defects, there was a reduction in the horizontal
dimension of the augmented hard tissue, comparing post-operative
and six-month measurements.
• The average time after tooth extraction was longer for noncontained
defects (7.5 months) compared with contained defects
(3.0 months).
Limitations
• Sample: no information about the smoking
habits of patients (only that heavy smokers were
excluded); use of the term “active periodontal
disease”, which does not follow the current
classification.
• Surgical procedure: wide time range after tooth
extraction, membrane stabilisation could have been
improved, and a high exposure rate after two and
four weeks in both groups.
• Main radiographical outcome variable might not
be adequate, as clinical measurements show less
resolution and are not ideal because three different
CBCTs were needed within six months.
• Unclear if the lack of statistically significant
differences in the results resulted from the sample
size calculation, which was merely empirical,
based on a superiority trial design. Only 35 patients
attended the short-term follow-up.
Conclusions & impact
• Immediately after wound closure, GBR with a soft-type BCP and
collagen block combined with a CM and fixation pins lead to superior
dimensions of augmented hard tissue compared to a particulate graft
plus CM.
• However, at re-entry, six months later, this dimensional stability
favouring the test group was not observed, and no differences were
found regarding augmented hard-tissue dimensions.
• The use of either a soft-type collagen-containing block or particulate
bone grafts in combination with a buccally tacked CM is not a
predictable alternative in reaching complete resolution of noncontained
peri-implant bone defects.
• Neither GBR with a BCP bone graft in a particulate presentation nor
supported with a collagen matrix creating a soft-type block seem to be
the ideal treatment option when treating non-contained bone defects
simultaneous to implant placement.